What is postural care?
Postural care is about protecting someone’s body shape, using equipment and positioning techniques.
Why do I need to know about it?
Children with neurodisabilities such as cerebral palsy are at risk of developing posture problems. This could include hip dislocation, spinal deformities and pain, as well as difficulties with digestion, eating and drinking.
Children who find it hard to move are most at risk of developing body shape distortions. This is because they often sit and lie in limited positions due to inactive and tight muscles.
How can I support my child?
By making postural care an integral part of your child’s care, you can maintain or improve your child’s health, body shape, comfort and physical ability. 24-hour postural care can help to balance muscle tone, improve your child’s sitting posture and tolerance, and help your child sleep better.
What activities can I do?
Our physiotherapists and occupational therapists can teach you how to understand positioning and correct your child’s posture. Postural care is achieved through:
Active exercise
Passive stretching
Regular change in positions
Use of dynamic splinting, such as Lycra suits
Use of special footwear, such as piedros
Use of orthotics such as Ankle Foot Orthoses (AFOs)
Use of arm/leg gaiters
Use of head supports
Provision and use of adaptive seating
Provision and use of standing frames
Positioning equipment to support your child as they lie down, including at night
Moving and handling techniques
By making sure your child is well positioned throughout the day and night, whenever possible, you can have a significant impact.
Other things to consider relating to postural care
Therapy can play an important role in postural care. Therapists can provide active and passive exercise programmes, seating assessments and advice, and night time positioning and sleep advice. Hydrotherapy and rebound therapy programmes are also available, and physiotherapists can advise on the use of standing frames and orthotics.
Medications and injections can be used to reduce spasticity. Your GP can advise you and make a referral to a neurologist if required.
Surgery is only used where spasticity is severe and cannot be managed by medical or physical measures. A neurologist, paediatrician or orthopaedic doctor would give further information.
The earlier the intervention, the better – but it is never too late to start protecting and restoring someone’s body shape. (Mencap, 2011)
What if I don’t support my child with postural care?
Failure to protect body shape can result in lots of health complications, including:
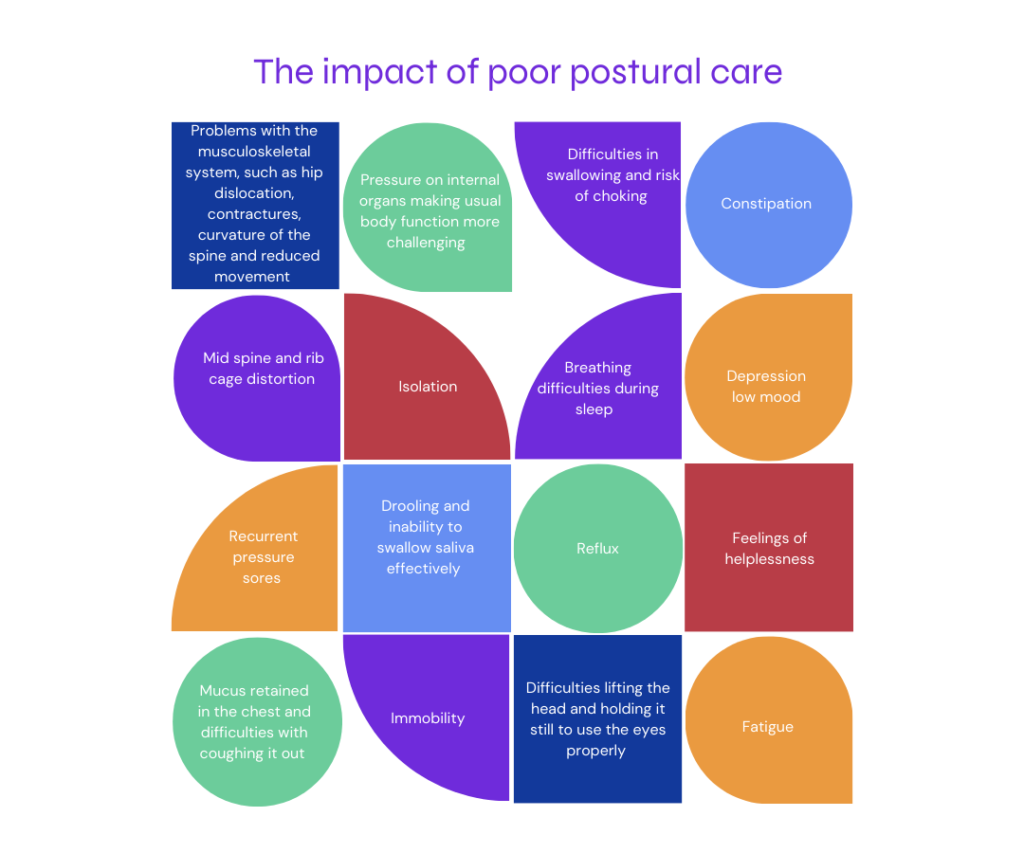
Mucus retained in the chest and difficulties with coughing it out
Drooling and inability to swallow saliva effectively
Immobility
Reflux
Breathing difficulties during sleep
Mid spine and rib cage distortion
Problems with the musculoskeletal system, such as hip dislocation, contractures, curvature of the spine and reduced movement
Difficulties in swallowing and risk of choking
Constipation
Pressure on internal organs making usual body function more challenging
Recurrent pressure sores
Fatigue
Depression / low mood
Isolation
Feelings of helplessness
Difficulties lifting the head and holding it still to use the eyes properly
These difficulties impact your child’s quality – and could impact your whole family. By providing positive postural care, you can reduce the risks, prevent issues arising and sometimes even improve your child’s condition.
